Necrotizing Enterocolitis (NEC) is a serious illness that primarily affects the intestines of newborn infants, with premature babies being particularly vulnerable. This condition involves inflammation that can damage the delicate intestinal tissue, and early recognition of its symptoms is crucial for timely medical intervention, which can significantly improve a baby’s outcome. This guide aims to provide parents and caregivers with essential information to help them understand and recognize potential signs of NEC Symptoms, especially in relation to infant feeding practices. Being aware of the symptoms and the factors that might contribute to NEC can empower caregivers to seek prompt medical attention when needed.
Table of Contents
Understanding Necrotizing Enterocolitis (NEC)
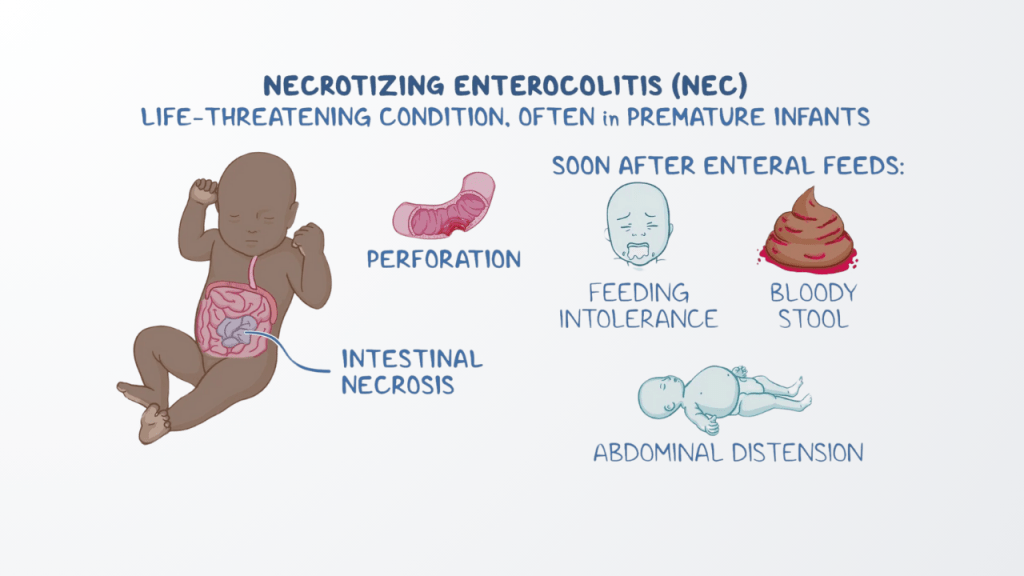
Necrotizing Enterocolitis is a condition characterized by inflammation of the intestines, potentially leading to the death of intestinal tissue. This primarily affects the large intestine, also known as the colon, and the small intestine. In severe cases, the intestinal wall can weaken, leading to a hole or perforation. This allows bacteria, which are normally present in the intestines, to leak into the abdominal cavity, potentially causing a severe infection.
While the exact cause of NEC remains under investigation, it is believed to arise from a combination of factors. Intestinal immaturity, particularly in premature infants, and the presence of bacteria are thought to play significant roles. The delicate and underdeveloped intestines of premature babies may react differently to bacteria and food, potentially triggering inflammation.
NEC predominantly affects premature infants. Studies indicate that NEC can affect between 2% and 5% of all premature infants, and this number can be as high as 10% in babies weighing less than 1500 grams (approximately 3 pounds, 5 ounces). It is recognized as the most common and serious intestinal disease among premature babies and a leading cause of death related to gastrointestinal issues in this vulnerable population.
While NEC is more prevalent in premature infants, it can also occur in full-term babies, although this is less common. In full-term infants who develop NEC, it is often associated with other health problems, such as congenital heart defects or events leading to low oxygen levels at birth. The higher occurrence in the most premature infants suggests a strong link between the immaturity of their intestinal systems and the risk of developing this condition.

The Potential Connection: Baby Formula and NEC Risk
Research has indicated a significant association between feeding premature infants with cow’s milk-based formula and an increased risk of NEC compared to those who receive human milk. Several studies have demonstrated a lower incidence of NEC in premature babies who are fed an exclusively human milk-based diet. In fact, a report by the U.S. Surgeon General highlighted that premature infants who are not breastfed are at a higher risk of developing NEC. This body of evidence suggests a correlation between cow’s milk-based formula feeding in premature infants and a greater likelihood of developing NEC.
Human milk offers several protective factors that may contribute to a lower risk of NEC. It contains substances that help the baby fight infection and aid in the maturation of intestinal cells, making it easier for premature infants to digest. Breast milk is also rich in bioactive proteins, immunoglobulins, and growth factors that are believed to protect against the development of NEC. Interestingly, research suggests that even partial supplementation of breast milk with cow’s milk-based formula might diminish some of these protective benefits. The components of breast milk appear to play a vital role in supporting the health and development of a newborn’s gut, offering a degree of protection against inflammatory conditions such as NEC.
Certain specific formula brands and products have been mentioned in research and lawsuits concerning their potential link to NEC. These include brands like Similac and Enfamil, along with their various human milk fortifier products. There is also some indication that formula with high osmotic strength might be a contributing risk factor. Furthermore, the way in which infants are fed can also play a role. Rapid or large-volume introduction of enteral feeds has been associated with an increased risk of NEC. However, the evidence regarding the optimal rate of advancement of feeds is not entirely consistent. While cow’s milk-based formulas, in general, have been implicated, it appears that specific formulations and feeding practices, particularly the rapid advancement of feeds, might further increase the risk in susceptible infants.
Recognizing the Early Warning Signs of NEC
Early recognition of NEC symptoms is vital for prompt intervention. Parents and caregivers should be aware of potential changes in their baby’s feeding behavior, abdominal appearance, and stool patterns. Subtle shifts in these areas can be early indicators of gastrointestinal distress.
Changes in feeding behavior might include poor feeding tolerance or a baby refusing to eat. Caregivers might notice that food seems to stay in the baby’s stomach longer than expected. An increase in the amount of fluid left in the baby’s stomach before the next feeding, known as increased gastric residuals, can also be a sign. Vomiting, especially if the vomited fluid is greenish in color (bile), is another important symptom to watch for.
Changes in the baby’s abdominal appearance can also indicate a problem. This might include a belly that looks bloated or swollen (abdominal distension). The baby’s abdomen might also feel tender to the touch. A change in the color of the belly, such as it appearing red, blue, or gray, can also be a concerning sign. In some cases, the loops of the intestines might even be visible through the skin.
Changes in stool patterns are another important indicator. This could involve the presence of blood in the baby’s bowel movements, making them appear bloody or dark. The baby might also experience diarrhea or, less commonly, constipation. The presence of blood in the stool is a particularly alarming sign that often indicates intestinal damage and should prompt immediate medical attention.
In addition to these signs, there are other systemic symptoms that might indicate NEC. These include the baby being unusually tired or less active (lethargy) , experiencing temperature instability, such as having a low or high body temperature , having pauses in breathing (apnea) , or having a slow heart rate (bradycardia). These systemic signs can indicate a more advanced stage of illness or a developing severe infection, requiring immediate medical evaluation.

Progression and Potential Complications of NEC
The early symptoms of NEC can be subtle and may gradually worsen over a period of hours or days. As the condition progresses, the inflammation in the intestines can intensify, leading to tissue damage and eventually the death of intestinal cells, known as necrosis. In severe cases, this tissue death can result in a hole or perforation in the intestinal wall. It is important to note that NEC can progress very rapidly, sometimes within a short period of 24 to 48 hours. This rapid progression highlights the critical need for caregivers to be vigilant for even subtle early signs and to seek immediate medical attention if they have any concerns.
NEC can lead to several serious and potentially long-term complications. These include:
- Intestinal perforation: A hole in the wall of the intestine.
- Severe infection: This can occur in the abdomen (peritonitis) and spread to the bloodstream (sepsis).
- Intestinal strictures: Scarring and narrowing of the intestines can develop as they heal.
- Short bowel syndrome: If a significant portion of the intestine has to be removed due to damage, it can lead to difficulties in absorbing nutrients.
- Liver problems: Prolonged use of intravenous nutrition, which may be necessary when the baby cannot feed normally, can sometimes lead to liver issues.
- Neurodevelopmental disorders: Infants who have had NEC are at an increased risk of experiencing developmental delays and other neurological issues.
- Death: In severe cases, NEC can be fatal.
The potential for these serious and long-term complications underscores the critical importance of early and effective management of NEC.
How Medical Professionals Diagnose NEC
Diagnosing NEC involves a combination of careful observation of the baby’s symptoms, physical examination, imaging studies, and laboratory tests.
During a physical examination, doctors will look for signs such as abdominal swelling, tenderness when the belly is touched, and any discoloration of the abdomen. They may also check for decreased bowel sounds, which can indicate that the intestines are not working properly, or if they can feel a mass in the baby’s abdomen.
Imaging tests play a crucial role in diagnosis. Abdominal X-rays are the primary tool used to confirm NEC. These X-rays can reveal characteristic signs like abnormal gas patterns within the intestinal wall, known as pneumatosis intestinalis. They can also show air in the veins of the liver or free air in the abdominal cavity, which suggests a perforation has occurred. Doctors may order a series of X-rays over time to monitor the progression of the disease. In some cases, an ultrasound of the abdomen may be used as an additional tool to assess intestinal movement, the presence of fluid, the thickness of the bowel wall, and blood flow to the intestines.
Laboratory tests also help in the diagnosis and assessment of NEC. Blood tests can be performed to check for signs of infection, such as an elevated white blood cell count, as well as to assess the baby’s platelet count, acid-base balance (metabolic acidosis), and other indicators of illness. Stool tests may be done to check for the presence of blood, which can be a sign of intestinal damage. The diagnosis of NEC is typically made based on a combination of these clinical findings, imaging results, and laboratory values, as there is no single test that can definitively diagnose the condition.
Causes of NEC
The exact cause of NEC is still not entirely understood; however, several risk factors have been identified. Premature birth is the most significant risk factor, along with factors like low birth weight, compromised immune systems, and a formula-fed diet. This brings us to an important aspect: the type of baby formula being used can influence the likelihood of developing NEC.
Recognizing NEC Baby Formula Symptoms
Identifying nec baby formula symptoms early on is vital to ensure your baby’s health. Here are some key symptoms to watch out for:
1. Abdominal Distension
One of the first signs of NEC is abdominal distension, which may appear as bloating in your baby’s stomach. If you notice that your baby’s belly looks swollen or feels hard, it’s crucial to contact your pediatrician.
2. Feeding Intolerance
If your baby is rejecting feeds or experiences vomiting especially after formula feeding, it may indicate a problem. Keep an eye on whether your baby seems more fussy or cranky after feeding.
3. Blood in Stool
Finding blood in your baby’s stool is a clear warning sign. It may appear as streaks or dark red spots. This symptom should prompt immediate medical evaluation, as it can indicate a serious condition like NEC.
4. Lethargy
If your baby seems unusually sleepy or unresponsive, this could be a symptom of NEC. Babies who are lethargic might not feed well and may become increasingly irritable.
5. Temperature Instability
Sudden fluctuations in your baby’s body temperature, particularly if they run a fever, can be a sign of infection or inflammation due to NEC.
6. Rapid Heart Rate
An increase in your baby’s heart rate is another symptom of NEC. Monitoring vital signs is crucial, especially in premature infants, who are at higher risk.
If you notice any combination of these nec baby formula symptoms, consulting a healthcare professional is imperative.
Conclusion
Necrotizing Enterocolitis (NEC) is a life-threatening condition that affects the intestines of newborns, particularly premature infants. Early detection of this illness can make a crucial difference in a baby’s recovery. Parents and caregivers should pay close attention to any changes in feeding behavior, abdominal swelling or discoloration, and unusual stool patterns, including the presence of blood. These symptoms may be early indicators of NEC, especially in babies who are formula-fed.
Because recent studies have suggested a potential link between certain infant formulas and NEC, it is vital that caregivers of formula-fed preemies remain especially vigilant. Prompt recognition and immediate medical intervention can greatly improve the prognosis for babies affected by NEC.
Understanding the risks, identifying symptoms early, and knowing when to act can empower caregivers to protect the health of their infants.
If your child has suffered from NEC after being fed cow’s milk-based baby formula, you may be eligible to take legal action.
Learn more about the NEC Baby Formula Lawsuit and your legal options